Children with Tracheostomy and Covid-19

Are children with tracheostomy at higher risk for contracting or transmitting Covid-19?
The coronavirus SARS-CoV-2 and resulting Covid-19 disease has resulted in a global health crisis. The virus that causes Covid-19 spreads mainly from person to person, typically through respiratory droplets from coughing, sneezing, or talking. Although people of any age can contract Covid-19, children are generally asymptomatic or have had more mild symptoms compared to adults.
Currently, there is no evidence that children with tracheostomy are at any increased risk of contracting or transmitting Covid-19. The tracheostomy tube itself does not determine if the child is extremely vulnerable. However, children with tracheostomy may not be able to cough and clear the airway as well as others, which could increase the risk of infection with a respiratory virus. There are some children with tracheostomy who also present with comorbidities and underlying medical conditions which can result in an increased risk for severe illness related to Covid-19. Similar to adults, children with obesity diabetes, asthma or chronic lung disease, sickle cell disease, or immunosuppression might also be at increased risk for severe illness from COVID-19 (CDC, 2020).
Children with tracheostomy breathe differently than an individual without a tracheostomy. The airflow is mostly directed in and out of the tracheostomy tube. Coughing is also redirected out of the tracheostomy tube. Since the tracheostomy tube is located below the level of the vocal folds, children with tracheostomy often have a weaker cough than an individual without a tracheostomy. The aerosols generated from the cough may then actually be less than aerosols generated by coughing by someone without a tracheostomy tube.
In the US and UK, there were few admission of children admitted with SARS-CoV-2 and very few admissions for tracheostomy or long term ventilated children.
The National Patient Safety Project has guidance for children with tracheostomy and long term mechanical ventilation. They recently have updated their guidance due to concerns of an overly cautious approach to the management of children with tracheostomy during the Covid-19 pandemic. There are fears this could disadvantage children by excluding them from their usual social or educational activities.
How to Reduce the Spread of Covid-19 to Children with Trachostomy
The virus that causes Covid-19 is mainly spread from large, short range respiratory droplets from coughing, sneezing or talking. It can occur from direct contact with an individual infected with the virus or indirectly from touching objects or surfaces in the environment that they have touched. The most common way the virus is spread is from these contaminated surfaces or hand contact, which is then transferred to the mucous membranes. This is why hand washing is so important.
During suctioning, to reduce exposure to staff, a heat and moisture exchange device can be placed on the tracheostomy tube. Suctioning can then occur through the tracheostomy tube to reduce the amount of aerosol spread. Appropriate PPE should be worn. See below for PPE with tracheostomy.
Here is a video on suctioning a child with tracheostomy.
For children with known or suspected Covid-19 it is important to reduce aerosol generating procedures, which are procedures that may result in a higher risk of transmission by inducing the production of aerosols. Personal protective equipment is very important to reduce the spread of Covid-19 when performing procedures that are aerosol generating, which are discussed in detail below.
Personal Protective Equipment
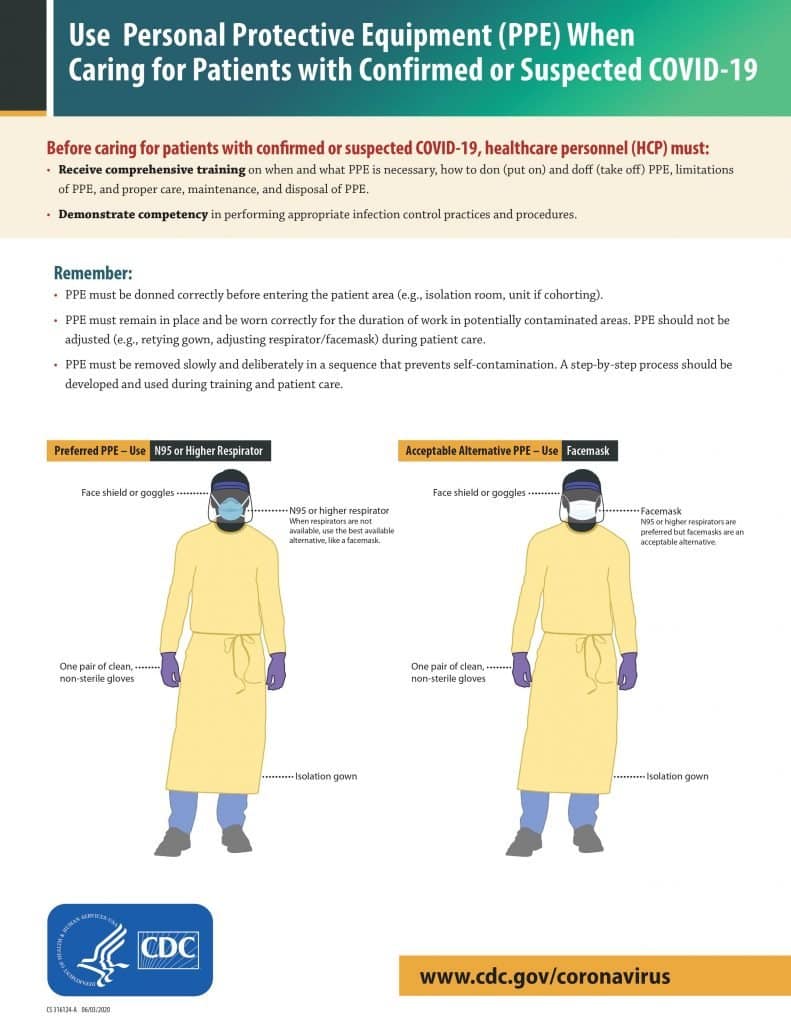
Personal protective equipment is equipment worn to minimize exposure to infection and minimize risks to the patient. PPE can include gloves, gown, face shield, and face masks depending on the risks posed to the caregiver by the child. The use of appropriate PPE is important in infection (such as Covid-19) prevention, as well as good hand hygiene.
There are different types of PPE that can be worn based on level of protection. For droplet precautions, PPE is for general protection against splashes and potentially infectious material. PPE for airborne precautions is a higher level of protection for higher risk patients and procedures.
The National Tracheostomy Safety Project recommends droplet PPE for general contact, cleaning equipment. They also recommend droplet PPE with aerosol generating procedures for patients with tracheostomy or long term mechanical ventilated children who:
- are well (asymptomatic), or
- have a recent negative COVID-19 test, or
- are managed in “green” clinical areas, or
- are managed in the community
PPE recommendations are evolving as estimated prevalence rates are changing. In the US, the CDC recommends airborne precautions for any aerosol generating procedure in a healthcare setting. In the UK, The National Tracheostomy Patient Safety Project states, “if the community prevalence is estimated to be below 2%, then we recommend that all asymptomatic (well) children can be managed with the simpler droplet PPE precautions for any aerosol-generating procedures.” Aerosol generating procedures for children with tracheostomy include noninvasive ventilation (NIV), bi-level airway pressure ventilation (BiPAP), Continuous positive airway pressure ventilation (CPAP), and respiratory tract suctioning (not including oro-pharynx suctioning).
For communities where the prevalence increases above 2%, the chance of an asymptomatic child being infected with coronavirus SARS-CoV-2 is increased. The National Tracheostomy Safety Project indicated that well/asymptomatic children who require potentially aerosol generating procedures to manage their tracheostomy are then managed with the increased protection with airborne precautions.
Aerosol Generating Procedures for Patients with Confirmed or Suspected Covid-19
For children with known or suspected Covid-19, as well as in a community with prevalence above 2%, the National Safety Project proposes airborne measures since the risks of exposure to the virus is higher. Reducing aerosol generation is important to reduce the risk. Appropriate PPE is important to prevent the spread of infection, particularly during tracheostomy care including tracheostomy tube changes, open suctioning, cuff care, and changes of the ventilator circuit. Closed suctioning is recommended when possible. Tubes with an inflated cuff also help to reduce the risk of aerosols since the aerosols are maintained within the circuit. Individual assessment is recommended because cuffed tubes prevent vocalization and can increase the risk of tube blockage.
General Modifications of Care for Children with Tracheostomy
It is recommended for established care to continue, but that aerosol generating procedures be kept to a minimum such as suctioning, cleaning/changing the inner cannula, reducing nebulized therapies. Children should wear a heat and moisture exchange (HME) if possible rather than an open tracheostomy tube.
Suspected or Confirmed Covid-19
If a child with tracheostomy or long term mechanical ventilation develops signs of symptoms of Covid-19, the doctor should be notified. Appropriate PPE is essential to prevent spread. Some children may be able to remain at home, while others may need hospitalization.
.
Summary
There is no evidence that children with tracheostomy are at any increased risk of contracting or transmitting Covid-19. There are evolving recommendations for PPE as the prevalence rates of Covid-19 reduce in certain communities. Allowing for less restrictive PPE for procedures such as suctioning for communities with a low prevalence rate of Covid-19 for children with negative testing or low risk, can allow for children with tracheostomy to get back to schools. However, PPE should still be worn. Emergency plans should be in palace with hospital specialists to provide information about what to do in an emergency.
For further reading, here is the Pediatric Tracheostomy and Tracheostomy Long Term Ventilated Care during the COVID Pandemic Updated Guidance: http://www.tracheostomy.org.uk/storage/files/Updated%20NTSP%20Paed%20Tracheostomy%20LTV%20during%20COVID_19%20Jan%202021.pdf
-

Trachie-O Framed poster
Rated 0 out of 5$30.00 – $120.00 Select options -
Sale!
Children’s Tracheostomy Book Hardcover | Trachie-O-Potamus’s Big Race
Rated 5.00 out of 5$24.99$21.99 Add to cart -

Trachie-o-potamus Toddler Tee
Rated 5.00 out of 5$21.99 Select options -
Finding Your Voice Songs for Kids with Trachs
Rated 5.00 out of 5$20.00 – $29.00 Select options












Responses