Laryngectomy and Coronavirus disease (COVID-19)

Introduction
COVID-19 is caused by a coronavirus called SARS-COV-2. The virus is spread from person to person, particularly after coughing and sneezing and through close contact (less than 6 feet) from one another. Coronavirus can also be spread by touching an object or surface with the virus on it, then touching the mouth, nose, eyes or stoma (in neck breathers) before washing hands. Symptoms of coronavirus include fever, shortness of breath, and coughing. Other symptoms include chills, headache, muscle pain, sore throat, and loss of smell and taste.
Those with laryngectomy may be suspectable to Covid-19 and other respiratory infections because of the change in anatomy following the laryngectomy procedure. Individuals with laryngectomy do not breathe through the upper airway (mouth and nose). Instead, breathing only occurs through the stoma to guide air into and out of the lungs. Therefore, in those with laryngectomy, air bypasses the natural defenses and air is not filtered and humidified by the nose. Thus those with laryngectomy are at risk of inhaling respiratory pathogens including the coronavirus directly into the lungs.
Laryngectomy patients are at risk for poor outcomes with coronavirus due to frequently present medical comorbidities. Commorbidities that are frequent in those with laryngectomy include chronic pulmonary disease, peripheral vascular disease, cardiac disease, cerebrovascular disease, diabetes, the underlying cancer history, and a propensity for atelectasis due to loss of upper airway resistance (Hess. MM, 1999). Many patients with laryngectomy are elderly and also have a history of smoking.
Please visit the CDC and WHO to stay up to date on the rapidly changing information for coronavirus.
Prevention coronavirus (COVID-19) in patients with laryngectomy
Those with laryngectomy may reduce their risk of contracting coronavirus through the following:
- Keep hands away from the stoma to prevent the virus from entering from the hands
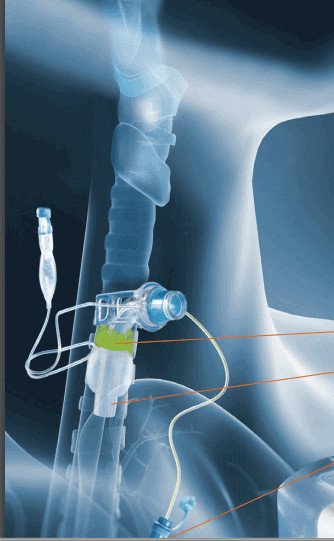
- Use of a heat and moisture exchanger (HME) with a bacterial or viral filter, at all times to cover the stoma. A baseplate is recommended (versus laryngetomy tube) for an adequate seal to the stoma to force air through the HME to minimize aerosolization. A hands free HME is recommended because it does not require touching when speaking. Those who use a regular HME (non hands-free) should wash their hands before touching their HME. An HME is important because it covers the stoma, creating a seal to prevent material from entering. In addition to filtration, it also helps with retaining heat and moisture. Infection rates and mortality were three times higher in non-HME users in comparison to HME users (van den Boer, C, 2014). Dispose the HME after community exposure. If an HME is not available/affordable, still cover the stoma with a mask (see below).
- Wear a face mask over the stoma, as well as the nose and mouth, as both areas can be a source of contamination. For the stoma mask, a surgical mask can be used by tying the upper mask strings around the neck and use additional extension string to connect the two lower mask strings together under the arms and behind the back. A facemask can reduce respiratory droplets that may contain the virus from entering the stoma and lungs. The mask can also help reduce any exposure of the individual wearing the mask to other individuals. Some face masks such as N95 can offer greater protection against smaller droplets. However, those with laryngectomy should check with healthcare professionals prior to wearing N95 masks as these masks may make breathing more difficult. While scarves and shirts are not as effective as surgical masks in reducing inhaled aerosol spread, they do provide some protection in reducing aerosol projection.
- Consider a hands free tracheal esophageal prothesis (TEP). If a hands free TEP is not available, the individual with a laryngectomy should be mindful of self contamination when touching the TEP device.
- Frequent hand washing and sanitation are important to reduce the spread of infection.
- Cover the stoma with a tissue when coughing and wash your hands after all expectorations. Those with laryngectomy are unable to cough up and expel secretions out the mouth or swallow secretions. Instead the cough is redirected out of the stoma.
- Hand washing is an easy and effective strategy to prevent disease. Hands should be washed for 20 seconds with soap and water.
- Avoid touching the nose, mouth, eyes or face (as well as the stoma).
- Stop shaking hands or kissing as a greeting. Social distancing from others is also a strategy to reduce the chance of infection. Follow all federal and local guidelines for isolation and quarantine recommendations.
- Clean and disinfect areas surface regularly as the virus may be viable on some surfaces for 24-72 hours.
Check out Dr. Itzhak Brook’s blog for more information about infection control prevention of Covid-19 for those with laryngectomy.
Coronavirus testing for patients with laryngectomy
Patients with laryngectomy have two potential sources for contamination, the stoma and the nasopharynx. Nasopharyngeal colonization can occur in a patient with laryngectomy even if there is no airflow occurs through the nose. Hand contamination and touching the face could lead to contamination of the nasopharynx. Tracheal colonization can occur through the stoma either through hand contamination and touching the stoma during stoma care, during phonation or from aerosolized exposure from close contact to an individual carrying the virus who sneezes or coughs.
For initial diagnostic testing for COVID-19, CDC recommends collecting and testing upper respiratory tract specimens (nasopharyngeal swab). CDC also recommends testing lower respiratory tract specimens, if available. Criteria for testing will vary by local supply and practices.
When obtaining specimens for coronavirus testing:
- PPE should be worn.
- Nasopharyngeal swabs can be obtained as usual.
- Tracheal swabs should be collected by minimizing coughing and aerosolization.
- No effort should be made to induce coughing.
- The laryngectomy tube, if present, should remain in place.
- If a Heat/Moisture Exchange (HME) filter is worn, this should be removed, mucous accumulated on the HME should not be utilized for testing as it may contain virus from an inhaled exposure that has not resulted in infection. The HME should be replaced following the sample to prevent any potential spread and aerosolization.
Infection control for patients with laryngectomy and coronavirus
If an individual with laryngectomy becomes infected with coronavirus, they carry a high risk of transmitting the virus to health care workers or the community due to their altered anatomy and typically increased secretions. There is a high risk of aerosolizing the tracheal secretions. Infection control strategies specific to patients with laryngectomy should be adhered.
Proper use of personal protective equipment (PPE) should be used, with only necessary careproviders entering the room of the patient. Patients should be presumed positive with COVID-19, until proven otherwise. Recommendations include N95 respirator and face shield or a powered air‐purifying respirator (PAPR), as well as a disposable surgical cap, gown, gloves, and consideration for shoe covers when evaluating any laryngectomy patient with unknown, suspected, or positive COVID‐19 status. Standard PPE, as defined by the Occupational Health and Safety Administration (OSHA), can be used for COVID‐19‐negative patients (Hennessey, M et al, 2020).
It is recommended to defer nasopharyngoscopy and tracheoscopy if possible as these are high risk aerosol generating procedures. When performing flexible tracheoscopy, attempts should be made to minimize mucosal stimulation and resultant coughing.
Tracheal suctioning may be performed through the stoma. Having patients self suction can allow for careproviders to leave the room to reduce the risk for spread. However, according to the New England Journal of Medicine, the virus (SARS-COVID-2) that causes coronavirus disease can remain infectious in the air for about 3 hours. After a few months post surgery, those with laryngectomy can typically expel secretions through the stoma without the need for suctioning. Coughing through the stoma helps to keep the lungs clear of organisms (bacteria, fungi, viruses including coronavirus) and other contaminants. During coughing, the stoma should be covered with a tissue and then hands washed after each expectoration. A suction machine should be readily available for an emergency such as a mucous plug.
Voice Rehab Devices Infection Control
Patients with laryngectomy also may use devices such as electrolarynx or TEPs. During the Covid-19 Pandemic it is recommended to wipe electrolarynx with alcohol pads after use.
TEP devices: An in vitro study on biofilm growth was conducted on various choices of the modern TEP voice prostheses, which concluded that use of silver oxide coating and Teflon as valve flap materials showed significantly less surface biofilm formation. For cleaning indwelling TEP devices, it is recommended to to use a dedicated brush to clear the device after meals. Soak the brush in disinfectants after use with one of the following methods: 70% ethanol for 10 minutes, 70% isopropylalcohol for 10 minutes, 3% hydrogen peroxide for 60 minutes. For nonindwelling TEP devices, it should be removed and soaked in disinfectants. Hands free TEP devices are available and reduce the need for contacting the stoma with the hands (Yeung, DCM et al, 2020).
Laryngectomy surgery during coronavirus pandemic
Emergency care for laryngectomy
Patients with laryngectomy are at high risk for improper care. Patients with laryngectomy do not have an upper airway to connect to the lungs. Breathing only occurs through the stoma located at the neck. Laryngectomy can often be confused with tracheostomy. In a tracheostomy, there is access to the upper airway. If there is any doubt if the individual has a tracheostomy or laryngectomy, the default emergency action is to apply oxygen to the face and the stoma for all neck breathers. Any oxygen applied to the upper airway can be removed in the case of a laryngectomy once this has been confirmed to be the case.
The National Patient Safety Project has developed an algorithm for emergency management of patients with laryngectomy.
Appropriate PPE should be donned during an emergency with an assumption that the patient may be infected with coronavirus during the pandemic. Full PPE is necessary as those with laryngectomy are at high risk for aerosolization.
Summary
There is no definitive data for the best care and management for those with laryngectomy and coronavirus. The laryngectomy procedure as well as those with an established laryngectomy are significantly aerosol generating. Therefore an increased risk of transmission is anticipated. Those with laryngectomy may be at increased risk for the coronavirus disease due to the bypassing of the filtering and hydration system of the nose. They may also be at increased risk of serious infection due to underlying commorbidities. It is important for individuals with laryngectomy to take steps to help prevent the spread of the coronavirus. The use of HMEs and covering the stoma can help limit exposure.
It is important to stay up to date on any changes that may be occurring. Please check the CDC website and WHO.
For more information, Dr. Itzhak Brook’s The Laryngectome Guide to Covid-19 Pandemic is available for free download as well as paperback.
Related Webinars:
References:
Brooks, Itzhak. The Laryngectomee Guide for Covid 19 Pandemic (2020).
Hennessy, M, Bann, DV, Patel, VA, et al. Commentary on the management of total laryngectomy patients during the COVID‐19 pandemic. Head & Neck. 2020; 1– 7. https://doi.org/10.1002/hed.26183
van den Boer C, van Harten MC, Hilgers FJ, van den Brekel MW, Retèl VP. Incidence of severe tracheobronchitis and pneumonia in laryngectomized patients: a retrospective clinical study and a European-wide survey among head and neck surgeons. Eur Arch Otorhinolaryngol. 2014;271:3297–3303. doi: 10.1007/s00405-014-2927-4.
Yeung DCM, Lai R, Wong EWY, Chan JYK. Care of Patients With a Laryngectomy During the COVID-19 Pandemic. Otolaryngology–Head and Neck Surgery. 2020;163(4):695-698. doi:10.1177/0194599820933185











Responses