Laryngomalacia: A Mother’s Journey

When I found out I was pregnant with my second child, I envisioned myself as being more relaxed than with my first. I would cherish each snuggle, nursing session, and tiny basket of laundry, as I was now aware how fleeting those first few months truly are. I remember the excitement driving to the hospital, knowing we would soon find out if our son would have a brother or sister. I remember walking into the unfamiliar hospital, blissfully unaware that not long after, these unfamiliar hallways and hospital rooms would be our second home.
Within the first few days of our second son’s birth, my motherly instinct knew something wasn’t right. Newborns are sleepy, but Vinny had very little awake time and rarely cried. He made tiny noises, like little squeaks. We trusted the doctor when he told us it was due to him being delivered via c-section, even though we never remembered our first son do the same. The nurses and doctors on staff (along with my husband and myself) became worried with the dramatic weight loss he experienced those first two days – just over 11 ounces. They were so worried, in fact, that we almost weren’t permitted to leave the hospital. When our pediatrician came by to check on Vinny on day 2, a Friday, she convinced the hospital staff that she would see us for weight check first thing the next morning and again on Monday. Knowing we had a dedicated pediatrician, hospital staff let us leave, and we took Vinny home. In hindsight, all the signs were there that pointed to an airway defect. We just didn’t know it yet.
Once we were home, those pesky little squeaks became louder and more frequent, earning Vinny the nickname “Little Goose.” He struggled to gain weight and by the end of his second week, we were visiting the pediatrician every other day for weight checks. It was then that our pediatrician mentioned a word I had seen among internet search results when I would look up “why is my newborn squeaking?” She wrote it down, along with the contact information of a pediatric ENT – “Laryngomalacia.” I left the office with instructions to make an appointment ASAP. Unfortunately, like most specialists, the wait time to be seen was about three months away.

Over the next six weeks, we continued to visit the pediatrician for weight checks and meet with lactation consultants. Vinny’s stridor (the official term for his squeaky noises) was becoming more severe, and we were noticing his ribs and neck being sucked in with each breath he took. At his eight-week checkup, our pediatrician decided Vinny couldn’t wait any longer to be seen by the ENT. He was only five ounces above his birth weight, was sleeping all the time, and his suspected Laryngomalacia symptoms were worsening. I was given strict instructions to head straight to the hospital for a direct admission, not even leaving the pediatrician’s office until we had a room number on the pediatric floor. I remember calling my husband, not being concerned. I figured we would be admitted, see the ENT, receive an official diagnosis, and be home the next day.
Upon admission, our nurse gave me a rundown of all the specialists our pediatrician had ordered for us to see. ENT, Gastroenterologist, Nutritionist, Occupational Therapist. The admission I expected to last one night, suddenly seemed like it would last a little longer. Within a couple of hours, Vinny was diagnosed as “failure to thrive” and an NG feeding tube was ordered. A hospital grade breast pump was wheeled into the room, and I was instructed to pump every two hours around the clock. My milk would now be fortified to increase the calories, in an effort to get Vinny to gain weight. I heard words like “malnourished” and “in distress” and suddenly felt a fear I never had felt before. Something was really wrong with my baby. It was more than noisy breathing, excessive sleeping, and slow weight gain. My husband comforted me as we watched multiple people poke and prod our not-even-8-pound two-month-old son.
Finally, around 8:30 that evening, the one specialist we had been waiting to see arrived. He introduced himself and let us know he would be performing a bedside scope on Vinny to check for Laryngomalacia. I held Vinny in my arms as the doctor inserted a long snake-like camera down through his nose, watching the findings on a screen. “Well, the diagnosis of Laryngomalacia is correct. Vinny will need a surgical procedure called a Supraglottoplasty.” Finally. We had the diagnosis. “So will you call us to schedule it?” my husband asked. The doctor responded with “No. I will book him an OR time for tomorrow. This can’t wait. Vinny can’t afford to wait.”
“Vinny can’t afford to wait.” Those words echoed in my head as the gravity of the situation set in. My baby needed surgery. What started as a normal Thursday, was now anything but. It was the day the line was drawn – before diagnosis, and after diagnosis. I remember barely sleeping that night. If I wasn’t pumping, I was researching NG tubes and Laryngomalacia and Supraglottoplasties. I was watching my tiny baby sleep in the big hospital crib, finding comfort in each squeak, knowing that meant he was breathing. I repeated the pattern for hours – pumping, researching, listening to his squeaks – waiting for them to call us down to the OR.
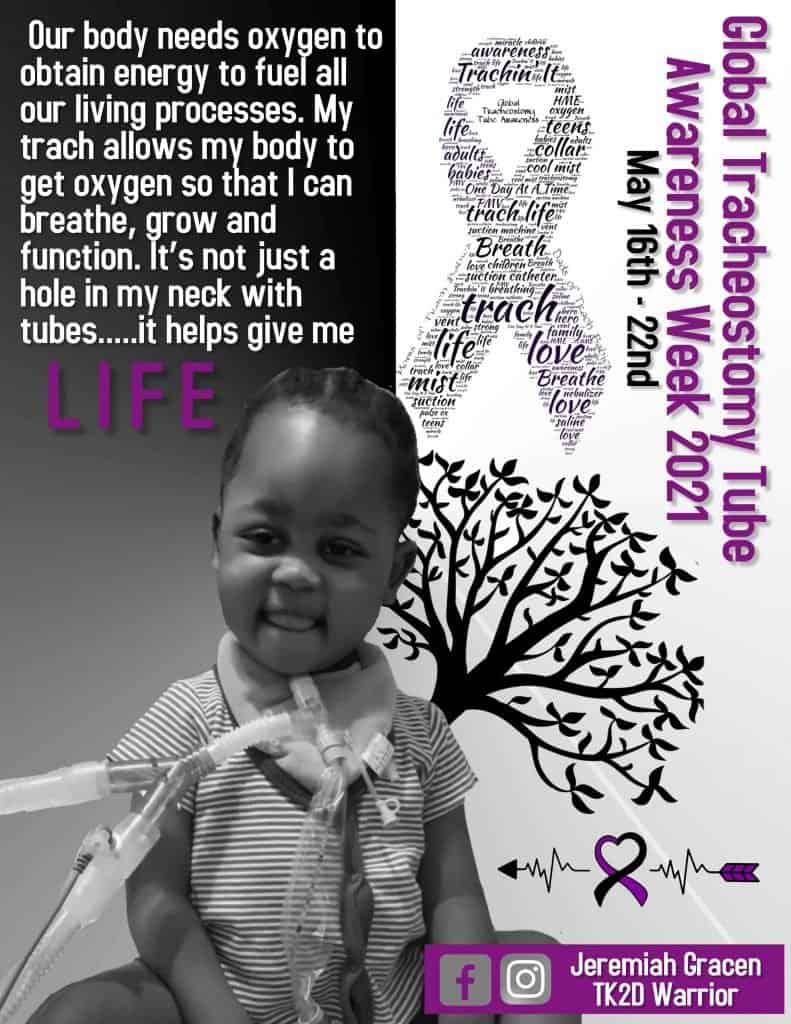
Finally, around 6 Friday evening, it was our turn. I sat in pre-op with my husband, rocking Vinny and staring at his perfect little face. I sobbed as I handed him over to the surgical nurse and anesthetist. My husband held me as we walked to the waiting room, where we were met by my parents, grandparents, and our older son. It felt like forever waiting for the ENT to come out and give us an update. Funny enough, the only other family in the waiting room that evening, was waiting for their infant to receive a tracheostomy. I remember thinking that even though I was scared, we were so lucky that our baby wasn’t that sick. Little did I know that in four short months, we would be in their shoes.
“We performed the Supraglottoplasty and placed his NG tube. Things went as expected. A nurse will come get you soon, to take you to the PICU for recovery. We will follow up tomorrow.” And just like that, we made it through Vinny’s first surgery and spent the night in the PICU. We were hopeful that he would begin to improve, grow, and thrive. The next morning, we were told that since he’d had a good night, we would be moved out of the PICU to a regular room. We would remain admitted “for a couple of days” to see if we could work on his weight gain. That couple of days turned into fifteen days, most of it spent back in the PICU following an episode of severe respiratory distress. We quickly realized Vinny wasn’t improving in the ways we had hoped.
The next two and a half months were filled with appointments, hospital stays, and tests. Vinny endured two more Supraglottoplasty surgeries, both of which didn’t yield the results his team hoped for. While we increased his team of specialists – which now included ENT, GI, Pulmonary, Neurology, Sleep Neurology, Plastics, Physical Therapy, Occupational Therapy, and Nutrition – Vinny continued to struggle. His list of diagnoses grew to include severe obstructive sleep apnea, Tracheomalacia, a Laryngeal Cleft type 1, hypotonia, severe GERD, and a mildly recessed jaw.
While recovering in the PICU after his third Supraglottoplasty, the idea of possibly needing a trach was brought up. Vinny was given one month to improve. Once again, we were told Vinny couldn’t afford to wait longer than that. The plan was, at the one-month mark, Vinny’s ENT would take him into the OR to check the status of his airway. Depending on what he found, along with Vinny’s progress during that month, the decision on a trach would be made in the OR. We went home determined that this third Supraglottoplasty would be the charm and Vinny would begin to breathe easy, grow, and thrive.
August 3, 2017 was the planned OR day. We arrived at the hospital knowing in our hearts that Vinny would leave with a tracheostomy. He hadn’t made much progress with his growth (at six-months old, he wasn’t even 12 pounds), and he was still struggling to breathe due to his Laryngomalacia and Tracheomalacia symptoms. He was missing milestones and still sleeping much of the time. Sure enough, we were right. When the ENT came to give us an update, he informed us a trach had been placed. Walking into recovery, I was flooded with so many emotions. I was happy the surgery was behind us, wondering how we even got to this place, relieved that he would hopefully begin to improve, and terrified of what would happen next. We weren’t prepared for “trach life” one bit.
That first day was a whirlwind. As they were getting him settled in the PICU, he woke up from the anesthesia, looking around. He looked terrified. The room was filled with nurses and hospital staff, hooking up monitors and poking and prodding him. He opened his mouth to cry… and there was no sound. The look on his face is a look I will never forget. Up until that point in his life, his only form of communication was his cry. Now it was gone. Tears were rolling down his cheeks, his face was bright red, his mouth was wide open, but there was no sound. I lost it. The amazing PICU nurses sat me down in a rocking chair and arranged Vinny, along with his wires and tubes, into my arms. As I rocked him, we both settled down. For the first time in a long time, we were both breathing easy.

The next day was full of visits from various hospital staff members, one of which was the PICU social worker. She handed us a packet of trach “dos and don’ts” and asked us to read it, she would be back to answer any questions. We read it and with each paragraph, our mouths dropped a little more. We would need a bigger car, as an adult wouldn’t fit between two car seats in the back of our Ford Escape to keep an eye on Vinny during car rides. What is a “Go Bag” and we need to carry how many different things with us at all times? Bathing looked different. Getting him dressed, especially in the beginning, looked different. What was trach care and what were trach changes? The list went on and on. The icing on the cake was when the social worker asked us how many nursing agencies we wanted to interview and what Durable Medical Equipment company we wanted to use? Nursing… in our home? Overwhelmed doesn’t even begin to cover how we were feeling.
We spent the next days learning how to care for Vinny and how to use his new “accessories.” We chose a nursing agency and graciously accepted my grandparents offer to trade our small SUV for their minivan, until our lease was up. A week post-op would be Vinny’s first trach change, performed by the ENT. In order to be discharged, one factor was being comfortable performing a change ourselves, and the first step was watching the ENT do it. Except I couldn’t watch. I hadn’t yet seen his stoma – or any stoma – and not knowing what to expect was too much. I expressed my overwhelmed stress to the ENT. I questioned why we hadn’t been better prepared prior to surgery. At that point, I didn’t know when I would feel comfortable taking Vinny home and I struggled with the idea that I no longer felt capable of caring for my own child.
Once again, the amazing PICU nurses stepped in. They worked tirelessly with us, exposing us to as many care scenarios as they could. They coached me through seeing Vinny’s stoma and stood by with orange juice and a chair as I performed my first trach change. After two weeks, everyone agreed we were ready to head home.
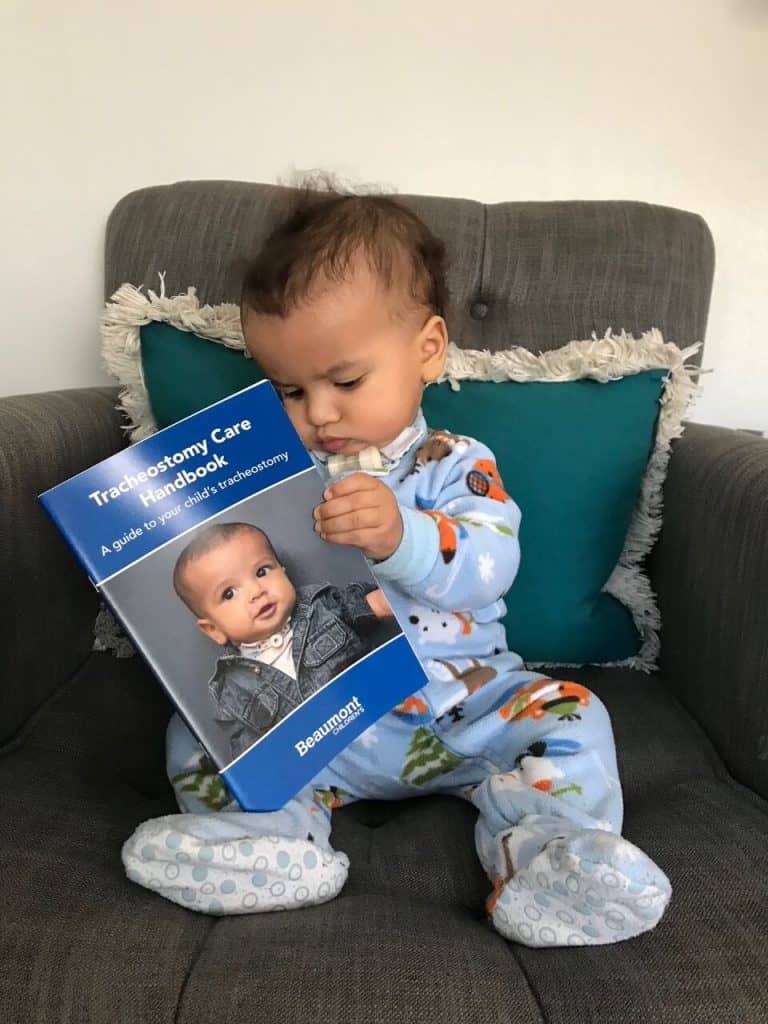
Life after that was busier than I could have ever imagined. Our small bungalow was filled to the brim with medical equipment and supplies. Our home became a revolving door to homecare nurses and multiple therapists each week. However, as each day passed, it became more and more clear that the trach had saved our son’s life. He was spending more of his time awake and his eyes lit up in a way they hadn’t before. The one thing that terrified me quickly became my security blanket. Our ENT even reached out to us, asking if Vinny would be their official “trach baby” and model for a caregiver guidebook. Because I spoke up about feeling unprepared, other parents wouldn’t have to be.

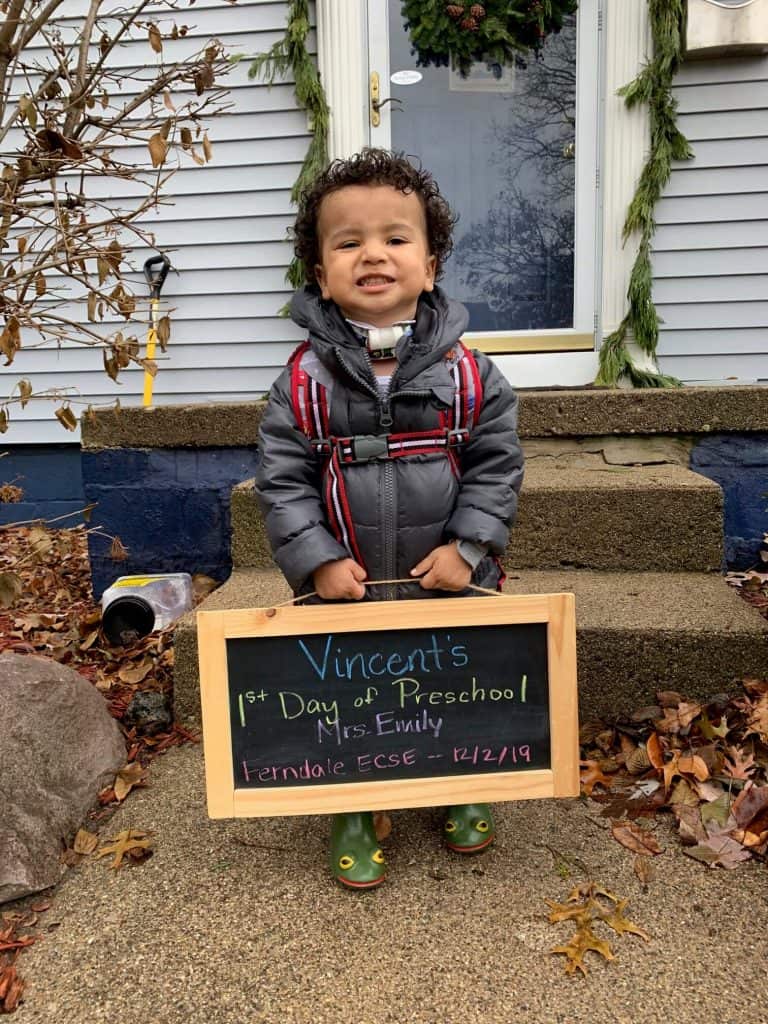
Vinny began to thrive. He grew. He started to meet milestones and he even found his voice! We began to hear the sweetest, tiniest coos coming from him. Each time we had something to celebrate, I thanked his trach. We learned how to adapt everyday situations so they would be safe for Vinny. For example, we filled his sandbox with rocks and marbles instead of sand. He even was able to start preschool in our district’s Early Childhood Special Education program, and he loved it!
Ultimately, the day came when Vinny’s medical team decided he was strong enough to consider decannulating. We began the process of capping and underwent the necessary evaluations and tests. With each step closer to decannulation, I found myself growing more and more anxious. Vinny’s trach had been part of him for over three years. That was three years of a safe airway, growing and thriving and learning. Three years we got to spend with our son, that we might not otherwise have had. It was also the only life Vinny knew, and he expressed quite a bit of anxiety and reluctance to decannulate. What happened if decannulating was the wrong decision?
April 30, 2021 was decannulation day. Following an OR scope and capped sleep study, Vinny’s medical team decided he was ready. After 1,366 days of trach life, Vinny’s trach was removed. Tears were shed – nervous tears mixed with happy tears. A new chapter of Vinny’s life was beginning.

It’s been six months of trach-free life, and I still have times where I forget he no longer has one! It’s been as much of an adjustment living life without a trach, as it was living life with one. Vinny’s stoma is closed, and I will always be thankful for that scar – it will forever remind him (and us) of all he has gone through and how strong he is. It’s a part of his story I never want him to forget. Although he is still considered to have Laryngomalacia and Tracheomalacia, he is now strong enough to live with his symptoms. His journey isn’t over, but that’s okay. We are grateful for his journey, and grateful for every breath.

-
Finding Your Voice Songs for Kids with Trachs
Rated 5.00 out of 5$20.00 – $29.00 Select options -
Sale!
Children’s Tracheostomy Book Hardcover | Trachie-O-Potamus’s Big Race
Rated 5.00 out of 5$24.99$21.99 Add to cart -

Tracheostomy Awareness T-Shirt Tracheostomy Tshirt | Star Trach Kids
Rated 0 out of 5$21.99 Select options -

Trachie-O-Potamus Coloring Pages
Rated 0 out of 5$0.00 Add to cart
Support Group
For caregivers of those with tracheostomy we have a new support group, Pediatric Tracheostomy Support group .
Coping with Laryngomalacia
Coping with Laryngomalacia is a non-profit which has a mission to provide support, strength, and education for families coping with laryngomalacia, tracheomalacia, bronchomalacia, and pharyngomalacia. Please visit for more information about laryngomalacia.










Responses