Mechanical Ventilator Alarms

If you work with ventilators than you have heard a ventilator alarm before. Ventilators incorporate monitors and alarms to alert care providers to changes in status of the patient or the equipment. Only individuals who are competent in ventilator management should change ventilator settings, including alarm silencing. There are differences in alarm set up and responses between different ventilators. Alarms can be visual, audible or both. Alarms can indicate important and potentially lifesaving problems. It’s important for clinicians working with ventilators to understand the reason for ventilator alarms, causes and troubleshooting to prevent an emergency.
To provide safe care to ventilated patients, the number of healthcare professionals who are allowed to adjust the ventilator should be limited. Setting alarms incorrectly can result in failure of alarms to activate when there is a problem with resultant morbidity and mortality. Respiratory therapists often have the training and experience to manage the ventilator and settings. Setting limits on volume, pressure and rate is every bit as important as the ventilatory settings themselves. Many institutions have policies requiring alarm settings to be set at a specific percentage of the ventilation setting.
Ventilator Alarm Issues
Issues cited in alarm related deaths include caregivers missing alarms. This can be due to ventilator alarm malfunction, although ECRI study determined that this was the case in only 2 of 119 cases it examined. Other reasons are that the alarm was not obvious or had been set inappropriately. “Alarm fatigue” is another issue where care providers become desensitized to alarms since they hear them often and many are false alarms and thus may miss true clinically significant alarms. There are not only ventilator alarms in acute care settings, but many other devices such as monitors, feeding tubes, infusion pumps, pulse oximeters, compression devices, beds, and many other devices. In one large study, there was an average of 350 alerts per bed per day and that in one ICU, the average was 771 alerts per bed per day. There are many “nuisance” alarms that do not require clinical intervention. Reducing the overall occurrence of nuisance alarms can help create a safer environment.
A policy and procedure on ventilator alarms is prudent to prevent adverse events. To our knowledge, there are no accepted standards regarding mechanical ventilation alarm parameters, monitoring frequency, and response expectations. AARC (2016) indicates that “Recommendations should support individualized settings in an attempt to create patient specific safety parameters. Ventilator alarm management policies should incorporate manufacturer specific alarm setting requirements, alarm functionality tests and an associated competency assessment. Standardization among manufacturers is non-existent, necessitating equipment specific training to familiarize staff with what alarm features are available, how to modify alarms, the sounds associated with various alarms including priority differences, how to extract alarm data, and reporting procedures for improving practice.”
Care providers should not solely rely on alarms as they may not always function correctly, and hypoxemia is typically the first clinical indicator. Ventilator checks are recommended. Also, for children requiring chronic home ventilation, an expert consensus recommends monitoring with a pulse oximeter rather than relying solely on ventilator alarms (AARC, 2016).
Think about what problems your institution has with alarms and the type of training being done about responding to alarms. Institutions should give considerable thought to alarms that should be activated, default limit parameter settings, and customizing alarms based on the patient’s needs. Some ventilator alarms can be transmitted to a care providers as a secondary alarm notification such as to a nurse call system, patient monitor, or connected to integrators and middleware.
A Ventilator is Alarming. What to do?
When an alarm sounds, any clinician nearby should attend to the alarm. Do not silence a ventilator until you have the situation under control and are aware of the reason for the ventilator alarm. Check the patient first such as their skin color, respiratory rate, level of consciousness, comfort. Make sure the ventilator tubing is connected appropriately. Check the patient’s vital signs including pulse oximetry. Try to determine the reason for the alarm by looking at the ventilator interface where most ventilators will display the most recent alarm. Review the last order and make sure the ventilator settings are the same ones on the ventilator.
If unable to quickly correct the alarm, or if the patient is in distress, initiate with bag-valve-mask ventilation to the tracheostomy and call for help. Bag valve and mask should be located in the patient’s room. Although for patients with Covid-19 we are trying to limit bag-valve-mask ventilation to prevent aerosolization, if the patient is in distress, it’s important to initiate.
An emergency algorithm was developed by the National Tracheostomy Safety Project.
Types of Ventilator Alarms
Common ventilator alarms include the following:
- High pressure alarms
- Low pressure alarms
- Low Volume alarms
- High Rate
- Low Rate (Apnea)
- High PEEP
- Low PEEP
High Pressure Alarms (High Peak Airway Pressure Alarms)
The physician or skilled clinician will set the high airway pressure limit. If the ventilator pressure exceeds the set pressure limit, an audible and/or visible alarm activates. When the ventilator pressure exceeds the set pressure limit, the ventilator immediately cycles into expiration and gas flow ceases. High pressure alarms are the most common ventilator alarms. Excessive airway pressures can cause barotrauma to the lungs.
Again always assess the patient first! Check the peak airway pressure. Normally the goal is below 35cmH2O, however this may not be realistic in a patient with ARDS.
Some possible causes for high pressure alarms include:
- Coughing is the most common cause
- Attempting to speak
- Patient-ventilator asynchrony where the patient exhales before inspiratory flow stops (can cause momentary increase in airway pressure)
- Kinks/bending in the ventilator circuit/biting circuit when on ET tube
- Water in the ventilator circuit
- Increased or thick mucus/secretions blocking the airway/mucous plug
- Bronchospasm
- Pulmonary edema
- Pneumothorax
- ARDS
Determine a plateau pressure by getting an inspiratory pause. Then determine the difference between peak and plateau pressure. If the difference is greater than 5cmH2O than increased airway pressure can be attributed to increased resistance such as from bronchospasm, anaphylaxis, ventilator obstruction (ie. Kinks in the circuit). If the difference between peak and plateau pressure is low, then increased airway pressure is likely due to decreased lung compliance and increased elastic work such as from pulmonary edema, pneumothorax, and ARDS.
If the patient is coughing/gagging or secretions, assess for the need for suctioning. If it’s pulmonary edema or pneumothorax, we want to consult the physician. If bronchospasm, consult respiratory or the physician.
Low Pressure Alarms (Low Tidal Volume Alarms)
The physician or skilled clinician will set the low-pressure alarm value. If the peak inspiratory pressure (PIP) decreases below the preset low airway pressure alarm limit, an audible and/or visible alarm activates. If the low-pressure alarm is set too low, especially below 10cmH2O, it may not alarm even with disconnect. Always assess the patient first!
Some possible causes for low pressure alarms include:
- Disconnection from the ventilator circuit or loose circuit/tubing connections is often the cause
- ET tube/tracheostomy tube displacement
- Air is leaking around the cuff of the tracheostomy tube
- The patient demands higher levels of air than the ventilator is providing
High and Low Rate Alarms
There may also be high and low-rate alarm settings. If the rate increases or decreases above or below the settings, an alarm will be activated. The low-rate alarm may also be called the Apnea alarm. Back up ventilation may be provided depending on the settings if there is a low rate alarm. Always assess the patient first!
Possible cause for the high-rate alarm include:
- Agitated or fatigued patient
- When autotriggering is present due to an incorrect sensitivity setting.
Possible causes of low-rate alarm include:
- Ventilators disconnect is the most common
- A sedated patient
- Impaired neuromuscular function who may not trigger the ventilator
- Patient is not triggering breaths
- Ventilator failure is also possible cause
If the ventilator fails, bag the patient with bag-mask ventilation and call for help for a new ventilator. If the ventilator is disconnected, reconnect the tubing. There are many places that the tube could be disconnected.
High and Low Expiratory Volume Alarms
High expiratory volumes may indicate an increased respiratory rate. Possible causes of high expiratory volume alarm include:
- Pain, anxiety
- Improper ventilator settings
Low expiratory volume will alarm with the volumes fall below a preset low volume threshold. This alarm is similar to a low-pressure alarm.
Possible causes of a low expiratory volume alarm include:
- Air leaking around the cuff
- Tracheal tube dislodgement
- Ventilatory tubing disconnect
High and Low PEEP Alarms
A high PEEP alarm occurs when the level of PEEP exceeds the preset PEEP.
The most common cause is when auto-PEEP or air trapping occurs. Autopeep is when air pressure remains in the lungs at the end of exhalation, which increases the work of breathing.
A low PEEP alarm occurs when the level of PEEP falls below a preset PEEP limit. The low PEEP alarm is useful to ensure the desired level of PEEP is provided to the patient.
The most common cause is when there is a leak in the cuff or ventilator circuit.
Inappropriate Inspiratory and Expiratory Time
Some ventilators may have a “inspiratory time too long” alarm that indicates a possible circuit obstruction or exhalation manifold malfunction. An “inspiratory time too short” alarm indicates that adequate tidal volume may not be delivered (in pressure-controlled mode) or that gas distribution in the lungs may not be optimal.
An “expiratory time too long” alarm may indicate apnea. “Expiratory time too short” alarm may indicate gas trapping.
Discharge Planning and Ventilator Alarms
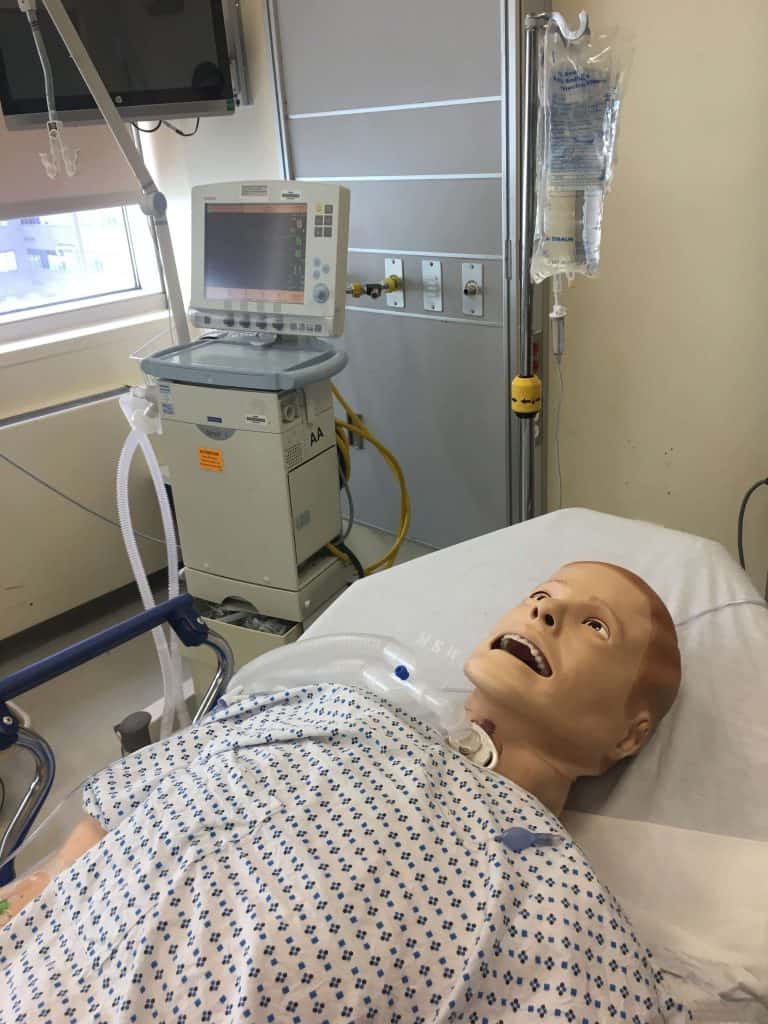
There are many alarms that care providers should be aware of to care for a patient with mechanical ventilation. Prior to discharge home, a caretaker should be able to respond to alarms and emergencies. American Thoracic Society Practice Guidelines for Pediatric Chronic Home Invasive Ventilation recommends care providers verbalize that ventilator alarms must be audible throughout the home, demonstrate an understanding of ventilator alarms and how to troubleshoot alarms (2016). Training and tracheostomy simulations such as with a tracheostomy manikin to return demonstration can aid in caretaker learning. Nurses and respiratory therapists who provide home care should also be knowledgeable about troubleshooting ventilator alarms.
Summary
Mechanical ventilators are complex machines, requiring proper training and competency prior to use in order to avoid patient harm. Inappropriate ventilator alarm changes can result in morbidity or mortality. The Joint Commission has indicated alarm safety as a patient safety goal back in 2005. Comprehensive and ongoing training and model-specific ventilator training for caregivers is prudent to reduce incidence of patient harm related to ventilator alarms. A committee should help set up a policy and procedure for alarm management. Care providers should document any changes to ventilator alarms.
Resources:
ECRI Institute. The Hazards of Alarm Overload: Keeping Excessive Physiological Monitoring Alarms From Impeding Care Health Devices. Available at: www.ecri.org. Accessed Monday December 27, 2021.
Jones K. Alarm fatigue a top patient safety hazard. CMAJ 2014 Feb 18;186(3):178
Sterni LM, Collaco JM, Baker CD, Carroll JL, Sharma GD, Brozek JL, Finder JD, Ackerman VL, Arens R, Boroughs DS, Carter J, Daigle KL, Dougherty J, Gozal D, Kevill K, Kravitz RM, Kriseman T, MacLusky I, Rivera-Spoljaric K, Tori AJ, Ferkol T, Halbower AC; ATS Pediatric Chronic Home Ventilation Workgroup. An Official American Thoracic Society Clinical Practice Guideline: Pediatric Chronic Home Invasive Ventilation. Am J Respir Crit Care Med. 2016 Apr 15;193(8):e16-35. doi: 10.1164/rccm.201602-0276ST. PMID: 27082538; PMCID: PMC5439679.












Responses