The Occupational Therapist’s Role in Tracheostomy

Occupational Therapist’s (OTs) play a crucial role in children with tracheostomy. OTs gets involved right from the start! OTs can receive therapy orders for the patient to begin moving with OT after the first trach change, which is usually about 7 days after a new trach is placed. Once medically cleared to move the patient, it is time for an assessment. We assess to see where a child is in their development and what skills they have as well as what skills they are working toward achieving.
Occupational Therapy Goals for Kids with Tracheostomy
During our assessments, we look at the child’s overall skill set including vision, hearing, gross motor movements, fine motor movements, socio-emotional development, and cognition. We also gather an in-depth understanding of the child’s home life, current therapy services, school services, and any specialized equipment they use. Once we determine a functional baseline and current needs (occupational profile), we come up with a plan alongside the family to advance the child’s skills and meet the family’s goals!
Although every child is different, we have found that most families and kiddos with trachs share these common goals:
- Attain highest level of mobility (sit, stand, move as independently as possible).
- Participation in everyday life skills such as dressing, grooming, and toileting.
- Engage in age appropriate play.
- Engage with peers and family members.
- Identify safe leisure activities.
- Obtain necessary equipment for home/school.
Occupational Therapy Treatment for Kids with Tracheostomy
These little superheroes have extra tubing making moving and playing a bit trickier. OT’s help to normalize movement and prevent bad habits!
As occupational therapists, we like to focus on the following:
Avoiding a Head Preference
Trach tubing usually lies to one side, discouraging full neck movement in that direction. We promote full neck movement to prevent tightness and allow for full engagement with the
Avoiding an arm preference/neglect
Since trach tubing usually lies to one side, kiddos typically prefer use of the more “free” We want to encourage symmetrical use of both left and right arms!
Avoiding a visual preference
- In the hospital, kiddos often develop a visual preference for the side of the crib/bed that medical staff and family approach most often. We want to make sure families and staff provide opportunities for visual exploration on both sides!
Facilitating quality movement transitions during play
- We have found that staff, family, and caregivers are rightly so nervous about moving children with a new trach! We are here to facilitate, educate, and encourage normalizing movement and movement transitions during play.
Facilitating quality movement
Oftentimes, kiddos with trachs are VERY SMART and develop their own creative ways to move. However, OT’s like to promote a more quality and symmetrical form of movement that will allow for advancing skills.
Encourage development of oral motor/oral sensory skills
Often, these kids with tracheostomy are not eating by mouth and do not have as many opportunities to advance oral motor skills or have oral stimulation. We provide as many normalized opportunities to advance oral skills as medically appropriate.
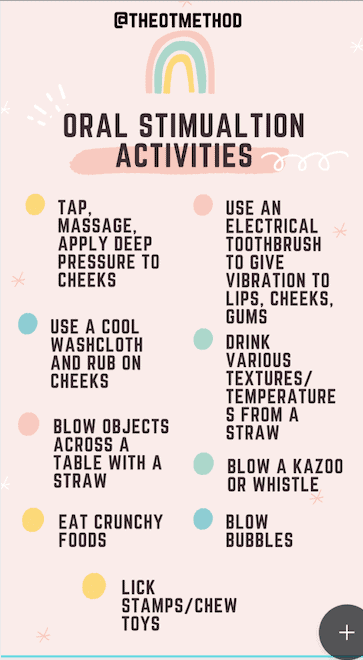
Interventions for oral motor development by a skilled occupational therapist may include the following:
- Tap, massage, or applying deep pressure to the cheeks
- Use of temperature such as a cool washcloth rubbed on the cheeks
- Blow objects across a table with a straw for uupper airflow (use of a speaking valve can help improve airflow)
- Eat crunchy foods (as tolerated per skilled clinician)
- Use an electrical toothbrush to give vibration to the lips, cheeks, gums
- Drink various textures/temperatures from a straw (as tolerated and deemed safe by the clinician and team)
- Blow a kazoo or whistle (improved airflow with a speaking valve if the child is able to tolerate)
- Blow bubbles (improved airflow with a speaking valve in the child is able to tolerate)
- Lick stamps/chew toys
Finding Your Voice, Songs for Kids with Trachs has activities to use where you can help increase oral airflow.
Providing Splints
We provide splints when medically necessary to facilitate movement and grasping. A trach alone does not warrant a splint! However, some kiddos with trachs have had long hospital admissions or additional diagnoses warranting the need for various splints to promote function!
Summary
The occupational therapist’s role in tracheostomy is to help meet the patient and family goals for mobility, safety, activities of daily living. We love educating families and letting them know that it is important and OKAY to move and play as children without trachs would. Specifically, tummy time, quadruped and rolling is not only okay, but ENCOURAGED!
Although this article pertains to the pediatric population, occupational therapists work across the lifespan.
About this author:
Sarah and Katie are both MSOT, OTR/Ls who are full-time acute care therapists in a children’s hospital. Their specialities are in pediatric oncology and pediatric cardiology. They love teaching about and advocating for occupational therapy and how it can be used in almost all settings across the lifespan! You can follow them on instagram @theotmethod
Related Products
-
Verbal Communication Options and Troubleshooting for Individuals with Tracheostomy and Mechanical Ventilation
Rated 0 out of 5$60.00 Add to cart -
Sale!
Children’s Tracheostomy Book Hardcover | Trachie-O-Potamus’s Big Race
Rated 5.00 out of 5$24.99$21.99 Add to cart -
Finding Your Voice Songs for Kids with Trachs
Rated 5.00 out of 5$20.00 – $29.00 Select options











Responses