Tracheostomy and Feeding Tubes

Overview of Artificial Nutrition and Hydration and Tracheostomy
A high percentage of patients with tracheostomy tube placement will require artificial nutrition and hydration at some point in their critical illness. In one retrospective review of trauma and acute care surgery patients, 79% underwent gastrostomy with tracheostomy as the concomitant procedure, whereas 21% received gastrostomy as a delayed procedure. Most patients (84%) who had a tracheostomy for prolonged or anticipated prolonged mechanical ventilation were receiving tube feeds at discharge (Djorak, J, 2019). Djorak et al. did not find a reduction in the length of stay for concomitant PEG. Other studies have shown benefits to the concomitant PEG including shorter length of stay, lower hospital costs and higher predischarge prealbumin (Nobleza, C., 2019).
Typically, patients are endotracheally intubated prior to a tracheotomy procedure being performed. When orally or nasally intubated, patients are unable to safely consume food or liquids by mouth. The endotracheal passes through the vocal folds, rendering inadequate airway protection. The epiglottis is unable to fully retroflex and the vocal folds are unable to close with an endotracheal tube in place, which are crucial in airway protection and swallowing safety. The endotracheal tube also provides a conduit for material to easily pass through the vocal folds and into the lungs. When material passes below the level of the vocal folds this is termed aspiration.
Aspiration is particularly dangerous for critically ill patients. If food, liquids, or bacteria from the oral cavity enter the lungs, there is a high likelihood of causing an aspiration pneumonia in a frail population.
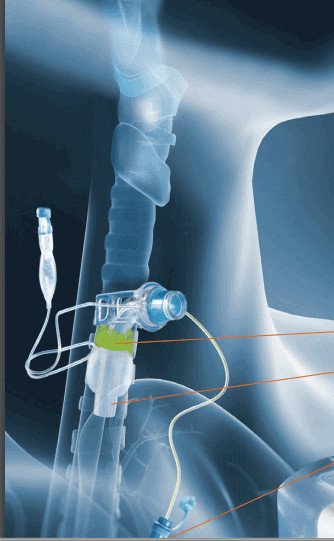
An alternative means of nutrition and hydration is required to sustain life during intubation and may also be beneficial for those with tracheostomy. The choices include nasogastric (NG), nasojejunostomy (NJ), percutaneous endoscopic gastrostomy (PEG), gastrostomy (G-tube) or jejunostomy (J-tube). Parenteral nutrition is also an option. Feeding tubes do not completely prevent aspiration. An individual may still aspirate oropharyngeal secretions or gastric contents when alternative means of nutrition are employed. Subglottic suctioning may be helpful in reducing microaspiration of secretions from above the cuff into the lungs. An endotracheal tube or tracheostomy tube with a subglottic suction port can be attached to an automatic intermittent suction device for removal of the secretions which can help to prevent ventilator associated pneumonia (VAP).
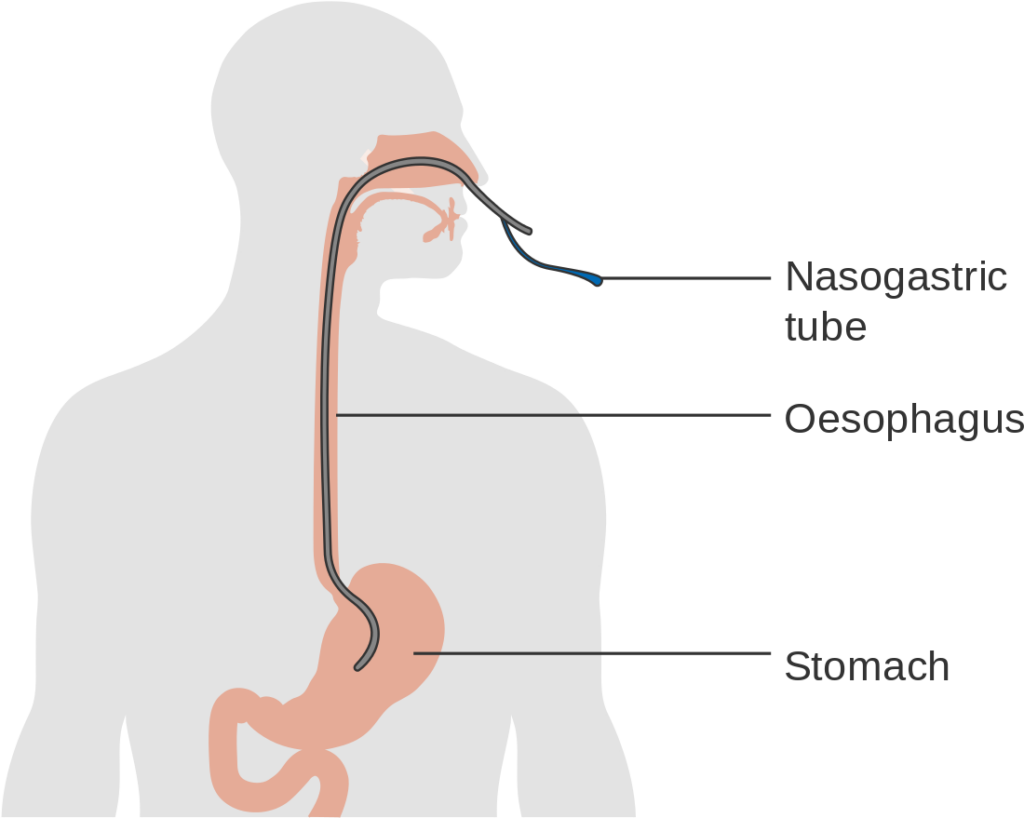
Nasogastric Tubes
A nasojejunal (NJ) tube is inserted into the nares and then into the esophagus, passes through the stomach and through the pylorus, and into the jejunum.
NG or NJ tubes are typically indicated for short term means of nutrition/hydration. Benefits of a nasogastric tube are that they can be inserted by nursing staff and can be easily removed. Care must be taken to ensure proper tube placement. A chest xray is recommended prior to begin feeding to ensure that the tube is inserted into the stomach rather than the lungs.
Gastrostomy Tubes (G-tube)

A gastrostomy tube (G-tube) is a feeding tube that is placed through the abdomen and into the stomach. A G-tube can be placed either surgically or percutaneously. A surgically placed G-tube is performed under general anesthesia in which a small incision is made in the abdomen for the tube to be inserted.
A percutaneous endoscopic gastrostomy (PEG-tube) is an endoscopically placed feeding tube that is placed into the patient’s stomach through the abdomen wall. G-tubes are indicated for long term means of nutrition/hydration. G-tubes are the preferred method of enteral feeding, unless there is upper gastrointestinal dysfunction, in which case post-pyloric feeding is recommended.
Jejunum Tubes (J-tube)
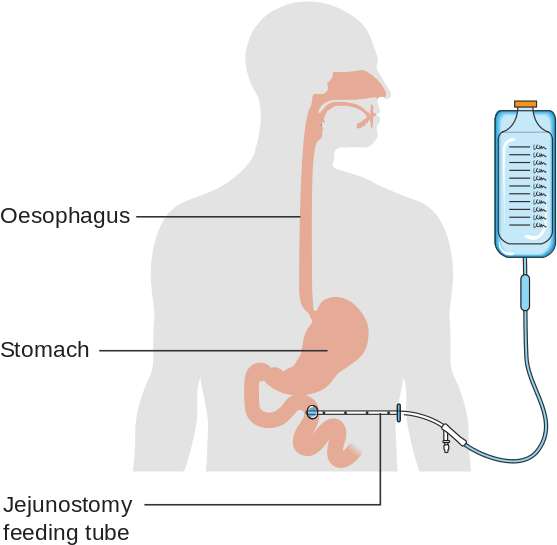
A jejunum tube (J-tube) is a surgically placed feeding tube that provides feeding directly into the jejunum. This is indicated for long term means of nutrition/hydration. A J-tube is typically placed in patients with an upper gastrointenstinal dysfunction or at high risk of aspiration from reflux.
Can patients with tracheostomy eat by mouth?
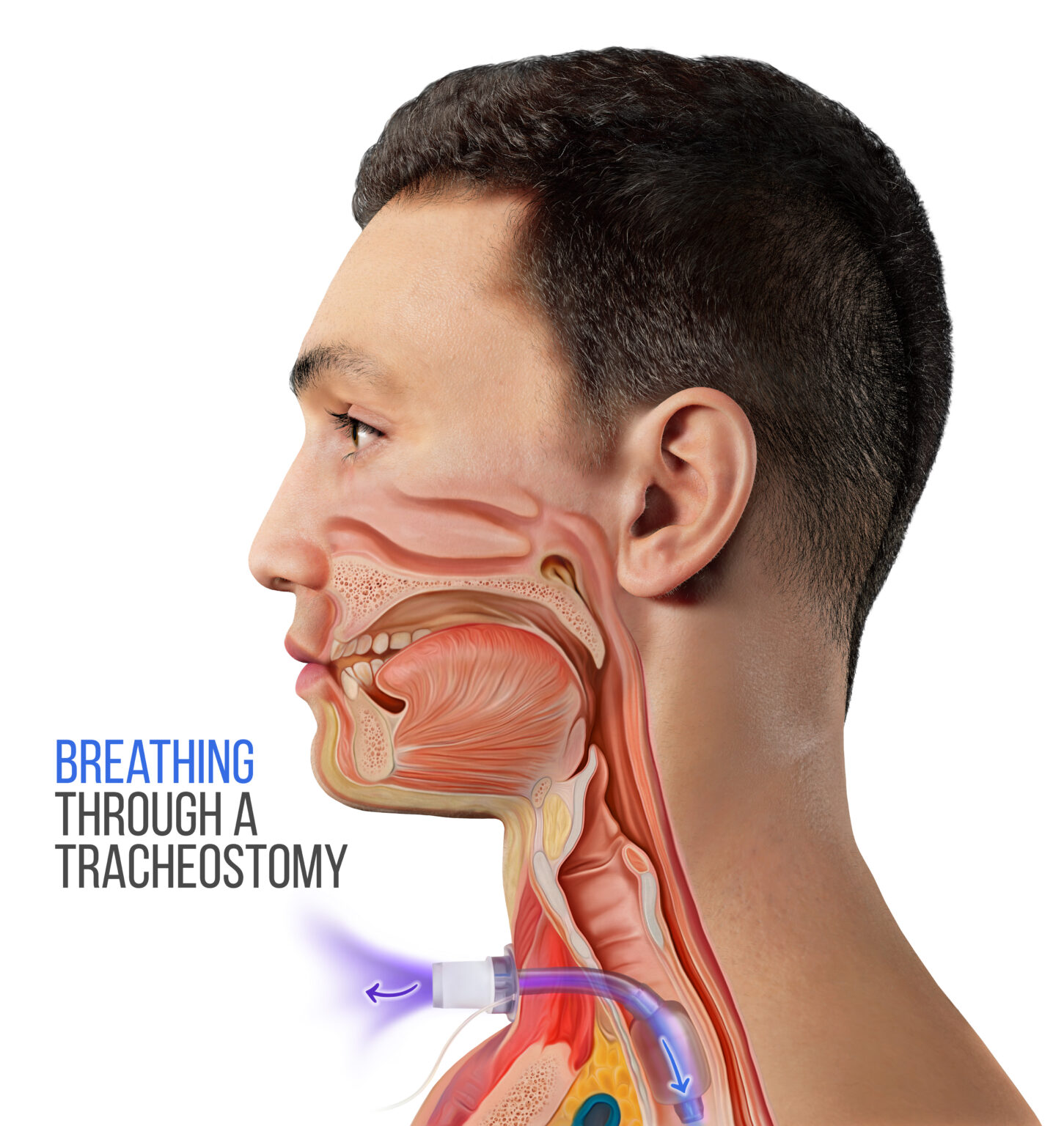
Once a tracheostomy tube is placed, there is a potential to eat by mouth. The endotracheal tube is removed when a tracheostomy tube is placed. The tracheostomy tube is placed below the level of the vocal folds. This allows for the vocal folds to provide some protection of the airway during swallowing.
Patients with tracheostomy are at high risk of aspiration with up to 50-86% aspiration rates with a majority being silent aspiration. Evaluation by a speech-language pathologist trained in dysphagia management for patients with tracheostomy is recommended prior to initiating oral intake. Tube feeding may be weaned and removed if oral intake is commenced and the patient is able to receive adequate nutrition and hydration by mouth.
See Swallowing Disorders section for more information on evaluating patients with tracheostomy for intake.
Summary
Those with tracheostomy and/or mechanical ventilation may benefit from an alternative means of nutrition and hydration. If the patient is medically stable, assessment by a speech-language pathologist is recommended to determine if the patient can safely eat by mouth following an instrumental swallow study.
Resources:
Dvorak J, Ridder D, Martin B, Ton-That H, Baldea A, Gonzalez RP. Is Tracheostomy Insertion an Indication for Gastrostomy Insertion?. Am Surg. 2019;85(5):518-523.
Nobleza COS, Pandian V, Jasti R, Wu DH, Mirski MA, Geocadin RG. Outcomes of Tracheostomy With Concomitant and Delayed Percutaneous Endoscopic Gastrostomy in the Neuroscience Critical Care Unit. J Intensive Care Med. 2019;34(10):835-843. doi:10.1177/0885066617718492










Responses